Challenges in the healthcare landscape, including clinician burnout, increased acuity, labor shortages, rising costs, shifting reimbursement and clinician compensation, have necessitated development of high-value hospital medicine (HM) programs with enhanced workflows. These programs aim to lower costs through improvements in productivity and skill mix while optimizing clinical quality, patient experience, throughput and access. Developing, implementing and sustaining such workflow and productivity enhancements require strong clinician engagement, competency and commitment.
Hospital Medicine Productivity Redesign Project Committee
Since 2019, TeamHealth’s strategically-focused Productivity Redesign Project Committee has been helping client facilities to optimize clinician productivity and engagement, while maintaining optimal levels of clinical quality, safety, patient satisfaction and throughput.
Structure and Function
The committee includes more than 70 recognized and experienced HM leaders. These leaders are from diverse backgrounds and include physicians, advanced practice clinicians (APC), operational personnel, data analysts and administrators from HR, finance, recruiting and legal. They act as subject matter experts and provide strategic guidance; develop the program structure, function and execution; and procure appropriate resources. The committee operates through five well-defined workgroups:
- Data Workgroup: Defines key productivity metrics and targets; develops robust analytical framework for real-time measurement and reporting; and provides business insights to facility leadership.
- Tools & Tactics Workgroup: Develops and refines custom toolkits to enhance workflow and culture and produces template communications for collaboration with local and regional operational teams.
- Compliance & Legal Workgroup: Reviews facility contracts and bylaws to ensure compliance.
- Clinical Compensation Workgroup: Reviews and enhances hospitalist compensation structure to better align with productivity and creates standardized plans to improve transparency and administration.
- Implementation Workgroup: Identifies and prioritizes facilities for implementation; oversees and strategizes change management; and trains Productivity Coaches and Productivity Super Coaches.
The committee’s organization encourages collaboration among the workgroups, peer-to-peer accountability and a defined structure for communications while allowing for specialization, innovation and focus on productivity improvement.
Resource Development
The committee executes its strategy with two high-value resources. First, a Productivity Coach is a high-EQ, high-performing clinical leader identified by the HM operations team. They collaborate with individual site medical directors and utilize the Productivity Toolkit to create tailored action plans to facilitate productivity improvement.
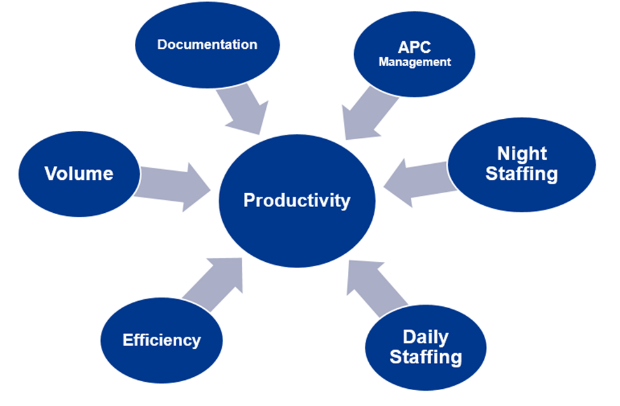
Secondly, the Productivity Toolkit is a detailed manual describing clinical and operational best practices. The toolkit is organized into six sections designed to address the key components of productivity performance. Each section provides best practices and tactics to improve productivity while simultaneously focusing on clinical quality, safety and clinician engagement.
Six Primary Sections for HM Productivity
Implementation
During implementation at sites, the team calculates ideal productivity targets based on their respective patient acuity and performs a gap analysis comparing baseline productivity to the ideal productivity target. This gap analysis dictates prioritization of sites. Productivity Coaches then collaborate with respective local and regional leadership at each program to create custom action plans.
Three scorecards enable real-time analysis of key productivity, quality and operational metrics. The report includes six key variables: productivity, length of stay (LOS), 30-day all-cause readmission rates, case mix index (CMI), percentage of discharge orders written before 11 a.m., Hospital Consumer Assessment of Healthcare Providers and Systems score (HCAHPS). The committee also monitors hospitalist engagement survey results and client retention rates. These scorecards enable cross-sectional and trend views at aggregate, facility and individual coach levels.
Analyzing the Program’s Effectiveness
To understand the effectiveness of the program and its impact on hospitalist productivity, the committee performed a retrospective analysis. The study aimed to discover the magnitude of change, the impact on key metrics and the effect of changes in CMI, given the program’s start during the COVID-19 pandemic.
Study Methods
Following a year of project planning, the program began implementation on August 1, 2020. The control, pre-implementation period consisted of 19 months starting January 2019 through July 2020. The post-implementation period consisted of 17 months from August 2020 through December 2021. All the elements of the program were in place, monitored and implemented during the post-implementation period.
The study defined productivity as encounters per adjusted day hour. Adjusted day hour included a weighted average of physician hours and 60% of APC hours, calculated per site. Overall, average productivity was compared between the control and post-implementation periods. Additionally, the six key performance indicators were measured for the same periods. Paired t-tests were performed and a p-value of <0.05 is deemed statistically significant.
Study Results
Average hospitalist productivity increased in 51 of the 56 facilities included in the study. The range of percentage improvement for all sites comparing these two periods is (-20.0%) to 39.7%. The aggregate change in productivity improved from a pre-implementation mean of 1.52 to a post-implementation mean of 1.64. Based on a matched paired t-test, the increase in mean productivity is statistically significant. One outlier high-acuity, specialty facility was not included in the pre- to post-implementation comparison for average productivity.
Summary Statistics for Differences Pre- and Post-Implementation of Productivity Redesign
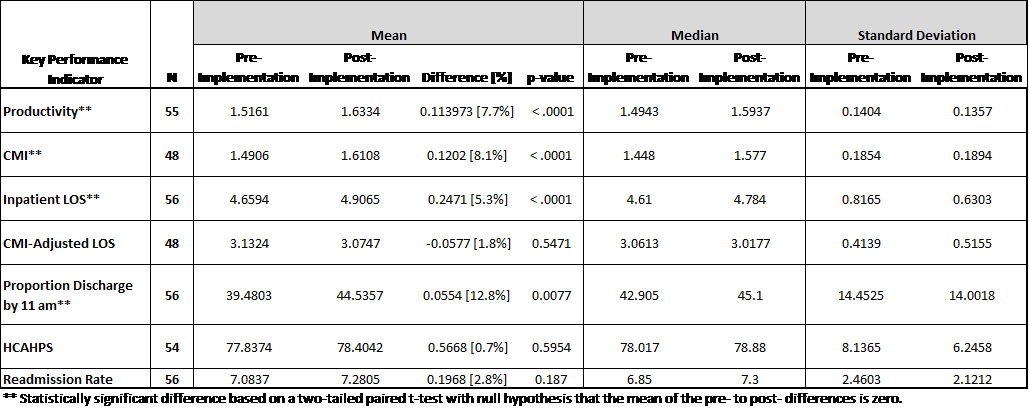
CMI-Adjusted LOS (acuity-adjusted LOS) showed a non-statistically significant increase of 1.8%. This suggested patient LOS was not a contributing factor, and that LOS and resource utilization were appropriate, based on increased patient acuity levels during the pandemic.
Evolving the Program
The project initially focused on 56 sites and is now being expanded to include all TeamHealth HM sites. There are ongoing efforts to enhance data analytics and forecasting related to hospitalist productivity. Optimizing the role of APCs is a new area of focus, and there are efforts underway to create tactics specifically focused on APC productivity.
The Conclusions
Hospital medicine productivity management is difficult, especially in recent times. As with any improvement, care must be given to avoid any negative effects on clinical quality, safety, patient satisfaction and clinician engagement. While results may vary among other hospitals and patient populations, this study concludes that TeamHealth’s Productivity Redesign Committee provided the necessary expertise and analytical framework to impact a positive change in hospitalist workflow at the sample facilities, driving productivity gains while maintaining historical levels of performance.
The findings support that organizational resource commitment and a culture fostering standardization, innovation and collaboration are successful in developing a high-value HM program. TeamHealth is a true partner in this space – offering the expertise, resources and experience to transform service line performance. Our teams aid hospitals and health systems in optimizing their resources to ensure high-quality care and operational excellence. Reach out to our team and discover the benefits of having the right partner for your facility. Download a PDF version of this white paper using the button below.